Understanding our ancestors’ genetic makeup to help us understand how our immune systems work today.
By Barbara Osypa, Contributing Writer
Only a few decades ago, the research conducted on the history and development of disease was limited to fossils, well-maintained records, and medical artifacts that withstood the test of time. Evolutionary anthropologists had barely breached the surface of what is now a vast reservoir of knowledge concerning how humans adapted to diseases throughout history. One key to revolutionizing the way that medical professionals understand human health is genetic sequencing. Although genomics, the study of genomes, may have come a long way since its origins in Mendelian genetics in the mid 19th century, it is a field that has only just begun to demonstrate its true potential. For instance, the Human Genome Project completed the monumental task of sequencing the entire human genome only 20 years ago (6). And even so, the full code was sequenced more recently, on April 1st, 2022, as the original project left approximately 8% of the genome unsequenced (6). Contrary to what the general public may expect, genetics is very much still a novel field of science in which very little is fully understood.
Today, with the aid of better technologies, researchers can confront several medical enigmas using genetics. Two recent discoveries in particular have had a significant impact on the scientific community and beyond.
The first found that a certain gene cluster is associated with the severity of COVID-19 cases. The variance in patients’ reactions to the virus is a unique and highly distressing characteristic of COVID-19 that still continues to baffle researchers. However, genetic analyses have provided some insight. Researchers from 23andMe, a personal DNA testing company, conducted a study that compiled and investigated over 1 million data sets of human genomes to find genetic variants that were associated with severe COVID-19 symptoms (1). In agreement with other similar studies, they concluded that variants in the gene cluster 3p21.31(1) affects the severity of COVID-19 symptoms. Questions have arisen, including why this connection exists or how this gene interacts with the COVID-19 virus. Although these questions remain unanswered, a corresponding study focused on the originations of the 3p21.31 gene cluster and found that it was inherited from our neanderthal ancestors. In collaboration with other professionals, Dr. Hugo Zeberg from the Max Planck Institute for Evolutionary Anthropology found that the gene has been passed down from an interbreeding event with neanderthals approximately 60,000 years ago (7). In an immense international effort of genome data collection for COVID-19 research, carriers of the neanderthal originated gene are claimed to have a three times higher chance of needing artificial ventilation if infected with the Sars-CoV-2 virus compared to non-carriers (7).
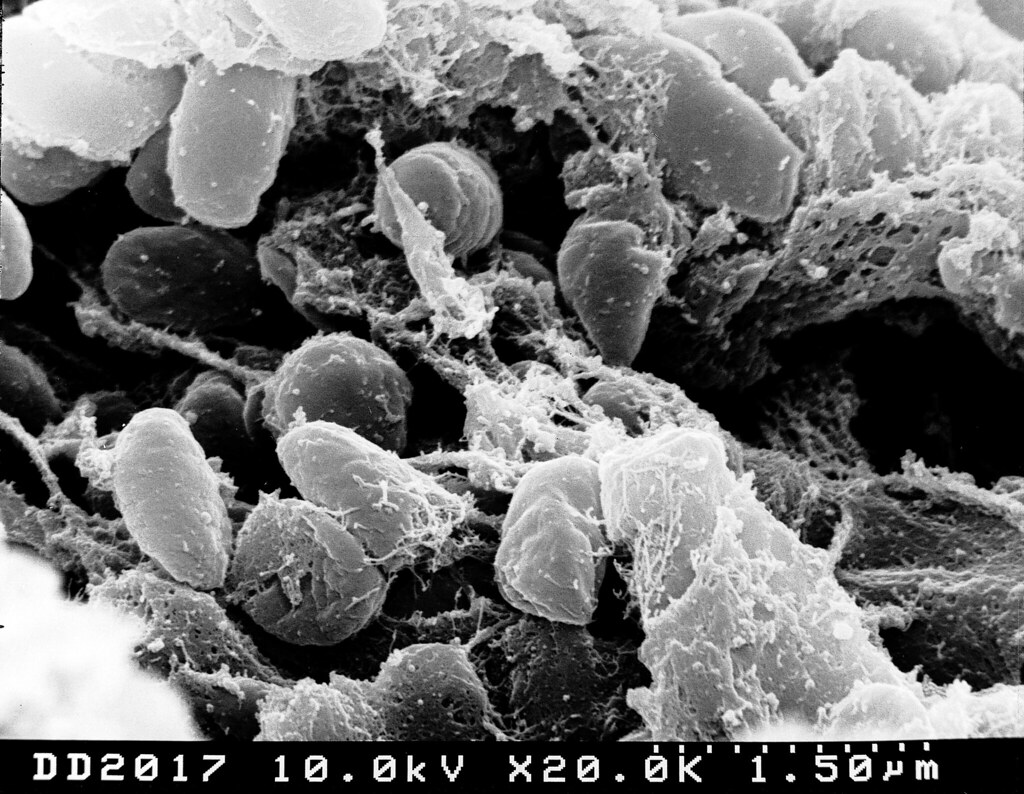
The other remarkable discovery was made much more recently, and a lot closer to home, by a team of researchers at McMaster University in collaboration with other international institutions. They determined that the bubonic plague had a role in the genetic evolution of how human immune systems react to diseases today (2). For context, the bubonic plague pandemic is the biggest natural selection event to have affected mankind – a fatality rate of above 50% was recorded (2). Signs of adaptation against the causative agent of the disease, a bacterium by the name Yersinia pestis, were traced in the study by collecting more than 500 DNA samples (2). As described in their published work in Nature (4), four distinct genes played a determining role in the likelihood of survival against the bubonic plague. Having two functional copies of the gene ERAP2 gave the individual a higher likelihood to survive and pass on their genes, while individuals with the non-functional copies were unlikely to meet such a lucky fate. ERAP2 genes influence the immune system’s cells capacity to fight off Yersinia pestis infections. In-laboratory experiments at the Pasteur Institute observed that the application of these genes in human cells enables macrophages to better deter Y.pestis growth (3). Presumably, descendants of survivors must have a better defense against modern diseases, yet it is the exact opposite. Those who contain the very same copy of ERAP2 that protects against the bubonic plague makes them more susceptible to autoimmune diseases like Crohn’s and rheumatoid arthritis (2).
What is especially exciting about these discoveries is that they demonstrate how advantageous genomics are in understanding the underlying cause of diseases plaguing our society. Previously, the obvious approach to treating disease was to pinpoint the Achilles heel in each disease and to target it with different therapies. As seen with many illnesses, this is not a permanent solution as viruses and bacteria can eventually overcome these treatments (e.g., the numerous COVID-19 variants and the corresponding vaccines). Or, in more perplexing cases such as Alzheimer’s, where the weakness of the disease is hard to find and treat (5), genetics can provide the missing links necessary to fight neurodegenerative illnesses. With genetics, researchers can now understand how the disease impacts each individual, at its very core. This opens doors to many new possibilities to understand, combat, and improve the way patients are treated.
Edited by Ella Iles and Ines Durant
REFERENCES
- Campbell, M. (2020, July 17). Study of Over 1 Million People Suggests Blood Type O May Protect Against COVID-19. Genomics Research from Technology Networks. https://www.technologynetworks.com/genomics/news/study-of-over-1-million-people-suggests-blood-type-o-may-protect-against-covid-19-340564
- Donovan, M. (2020, August 19). Black Death shaped evolution of immunity genes, setting course for how we respond to disease today. Brighter World; McMaster University. https://brighterworld.mcmaster.ca/articles/black-death-immunity-genes/
- Institut Pasteur. (2022, October 27). The Black Death shaped the evolution of immunity genes, setting the course for how we respond to autoimmune diseases today, researchers find. Institut Pasteur; Institut Pasteur. https://www.pasteur.fr/en/press-area/press-documents/black-death-shaped-evolution-immunity-genes-setting-course-how-we-respond-autoimmune-diseases-today#:~:text=The%20scientists%20discovered%20that%20versions
- Klunk, J., Vilgalys, T. P., Demeure, C. E., Cheng, X., Shiratori, M., Madej, J., Beau, R., Elli, D., Patino, M. I., Redfern, R., DeWitte, S. N., Gamble, J. A., Boldsen, J. L., Carmichael, A., Varlik, N., Eaton, K., Grenier, J.-C., Golding, G. B., Devault, A., & Rouillard, J.-M. (2022). Evolution of immune genes is associated with the Black Death. Nature, 611, 312–319. https://doi.org/10.1038/s41586-022-05349-x
- Korczyn, A. D. (2012). Why have we Failed to Cure Alzheimer’s Disease? Journal of Alzheimer’s Disease, 29(2), 275–282. https://doi.org/10.3233/JAD-2011-110359
- National Institutes of Health. (2022, April 11). First complete sequence of a human genome. National Institutes of Health (NIH). https://www.nih.gov/news-events/nih-research-matters/first-complete-sequence-human-genome#:~:text=The%20Human%20Genome%20Project%2C%20completed
- Zeberg, H., & Pääbo, S. (2020). The major genetic risk factor for severe COVID-19 is inherited from Neanderthals. Nature, 587, 610–612. https://doi.org/10.1038/s41586-020-2818-3